Heads of Service
Heads of Service webinar videos
The British Academy of Audiology hosts regular Heads of Service webinars. The sessions are designed to share key guidance and information and act as a forum to engage, discuss and share what we are all doing in our departments and to support each other during the Covid-19 outbreak.
Please keep an eye on the events pages for the next webinar, or email: victoria@baaudiology.org to be added to the registration email list. Previous webinars can be viewed below.
Also included on this page are support documents for different areas highlighted during our heads of service discussions. Remote Programming, supporting the Health and Wellbeing of staff, an overview of Essential Routine Services and information on Registration, Redeployment and Transferable Skills are all covered below.
FAQs from 4th June webinar
During the webinar on 4th June, there was a steady flow of questions and answers. We have categorised them below. Links to specific guidance and resources are also included. Please let us know if you have further information and knowledge about any of the areas covered.
Questions
- With regard to air calorics has it been confirmed that air calorics are okay with appropriate PPE?
- What about water calorics, please?
- Can we do PTA, imps, fittings on people with perforations?
Shared comment/opinion
The joint guidance released on Monday 1st June references caloric PPE in appendix 7. You can download the guidance here.
Quote from Professor Peter Rea – received post-webinar re Q3 above: “I have been working with colleagues tonight on (yet another) research project looking at what material comes out of a wet ear with suction which would be relevant to this. A thought to reflect on is if we do a suction, audiogram, or fitting on a wet ear that has pseudomonas we can all smell the pseudomonas. As such it seems reasonable to assume that if a bacteria can be produced in this way from the ear, so can a virus. What we don’t know is whether COVID-19 infections are associated with the virus in the middle ear. I have just about got funding to culture middle ear mucosa from infected patients (a complex project I can explain another time if we get it done). If they are then testing a wet perforation or a wet cavity my opinion is there must be significant risk in a patient with COVID-19. I would not advise doing that. This is my opinion and cannot at present be based on science. For a dry mastoid cavity, I see no problem in contrast as any virus should, in theory, be behind the TM. You are right cough is not considered an AGP by PHE. However, it would be most unwise to get in the way of a cough of an infected patient. Having the patient wear a simple mask greatly reduces aerosol release and I would strongly recommend your members do this during both testing and fitting until the prevalence of infection is lower.”
Resources
Aerosol Generating Procedures (AGPs) – NHS National Services Scotland
Assessing the evidence base (AGPs SBAR) – NHS National Services Scotland
Questions
- How do I clean the booth & fabric walls?
- Has anyone had advice from IPC on Hessian if not using air-con?
Shared Comment/opinion
“We are using Chlor clean on hard surfaces as advised by out Trust and Clinell.”
The Quiet Star guidance linked below is comprehensive and covers most types of acoustic environment surface cleaning.
Resources
Questions
- What is the guidance on the use of Air Cons?
Shared Comment/opinion
The Health and Safety Executive have published guidance:
Air conditioning
The risk of air conditioning spreading coronavirus (COVID-19) in the workplace is extremely low.
You can continue using most types of air conditioning system as normal. But, if you use a centralised ventilation system that removes and circulates air to different rooms it is recommended that you turn off re circulation and use a fresh air supply.
Resources
Covid-19 and the risk from air-recirculation in buildings
Secondary care: document of preparedness
Questions
- Linking to the infection control questions any guidance on extraction fans that we use for drills and buffers are they being used by other services – is the risk of these known?
- Are earmoulds being Chlor Cleaned prior to adjustment?
- Is anyone using an earmould scanner?
Shared comment/opinion
“Grinding and buffing will kill the virus as it generates >60 degrees temperature.”
“Re: buffing machines – I’m about to visit my maxfax dental lab to see what they use as they have single-use mops and polishing whereas I suspect most audiology depts use large mops & stones which are NOT changed each time a new mould is modified. That needs to stop immediately! For interest, maxfax use polishing kit to polish the likes of “eyes” so they are cleaned pre-polishing but mainly because they are likely to be slightly “dirty.”
Questions
- What approach are services taking with the newborn screening of infants of confirmed Covid-19 mothers? Are these infants being screened in maternity units and what IPC precautions are being applied?
- What if patients accept an appt. for diagnostic Audiology then DNA? Do we follow local DNA policy and discharge?
- The current NHSP document says babies can be screened up to 6 months. Presumably, we can make local arrangements to see the babies behaviourally if they have declined the screen?
Shared comment/opinion
“Assigning a parent to decline consent due to risk issues seems unfairly harsh. They may well wish to have assessment but only when safe I am not comfortable with complying with this advice.”
“Barts Health NHSP/Audiology Lead here – we are not screening COVID+ Mums. Our service is time-limited yes but so few are now confirmed on admission, there’s no need to offer screening on an inpatient basis.”
“Surely if parents want the screen later due to Covid anxieties they will get a GP referral for behavioural anyway so why not TFU.”
“If Covid we wait as not all screeners can go into COVID areas with personal risks assessments.”
“We have never stopped screening or diagnostics and there are VERY few declines due to Covid.”
“I’m not finding any of our mothers deferring OP screening. They’re all keen to come out and have baby screened. They’ve often isolated since birth. They need to be informed better about the level of risk of attending a community newborn appointment. They’re unlikely to miss their postnatal/breastfeeding follow-up appointments in the community.”
Resources
Jason Smalley is happy to answer emails directly and can be contacted at Jason.Smalley@nuh.nhs.uk
Questions
- I’ve heard that paediatrics get different Covid symptoms, is there any evidence of this?
- Is there any specific guidance for PPE when conducting otoscopy and impressions for young children who may not be compliant (held by parents), crying, coughing etc
- What are paediatric departments doing about the fact that grommets are not being routinely fitted so referrals for hearing aids have gone through the roof (certainly for us!) as ENT is referring a lot of transient glue ear cases to Audiology to potentially aid instead of grommets? Any solutions anywhere?
- Re children’s hearing aid follow-ups – is everyone sticking to 6-8 weeks for new fittings? Or extending the time between appts? Perhaps doing telephone follow-ups. And should under 5s still be seen every 6 months?
- With new baby fittings, are you having any difficulties with the EM’s coming back within a good timeframe? Concerned that if we start fitting babies, the EM’s are going to be a big problem.
Shared comment/opinion
“Children are less likely to be tolerant of wearing a mask when seen in outpatients or on the ward. They are more likely to cough and sneeze uncontrollably. They may not maintain a 2m distance from others, and may not be able to be fully controlled by their parents. This increases risk of viral transmission to others in the outpatient and ward environment. Availability of PPE should take this into consideration”
“The overall population risk of paediatric infection is low. However, while it was previously considered that children do not suffer severe consequences of infection, there is increasing awareness of a group of Covid infected children who develop a variant of toxic shock syndrome.
The sensitivity of antigen testing in children is low as:
• it is more difficult to get a high-quality swab on a child as the child is likely to be less
compliant
• viral clearing from the URT in a child is thought to be quicker”
Resources
Questions
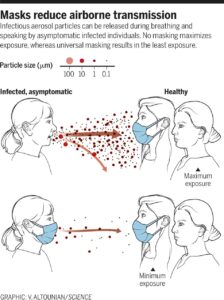
- Our organisation thinks that we shouldn’t be providing masks to patients as there is no evidence that it helps? We are obviously not ready to see patients without both parties wearing a mask. Any advice?
- Following Government announcement about all Hospital staff wearing masks – what do you think?
Shared comment/opinion
Note: answers from 4th June:
“So far. Patients all have health questions, temp check and are “fit and well”. It’s the same across the rest of the organisation. Also, Covid rates in the community here aren’t very high, which I think informs everything.”
“We are asking people to bring and wear a cloth mask.”
“We’re following Trust IPC guidance – not having patients wear a mask.”
“Our trust advice is that all patients/and children over 2years should wear face masks that they bring themselves. we have to supply if they haven’t bought them.”
6th June
Following the Government face masks in the NHS announcement, BAA does recognise the importance on the transmission risk but has raised concerns on the negative impact on communication and procurement challenges. A letter has been sent to Matt Hancock from BAA and template letter written for audiologists to send to their local MP.
Resources
Government face masks announcement
BAA letter to Rt Hon. Matt Hancock
Scotland, Wales, Northern Ireland member letter
How to write to your parliamentary representative
Face masks for the public during Covid-19 crisis
Reducing transmission of SARS-CoV-2
The role of community wide wearing of face mask
Questions
- Is the information sheet about the Impact of Facemasks available to download anywhere?
- Where can you get clear facemasks?
Shared comment/opinion
“Paul White at Addenbrookes he’s a clinical engineer.”
“I can send an unusual design to Paul – which doesn’t mist up or get too hot.”
“We got our Trust to order a lot of whiteboards for the wards to aid communication.”
“There is a clear mask made in Portugal that evidently is CE marked.”
Resources
Questions
- Are there any departments that are seeing patients face to face who are not priority cases?
- What are the criteria to see ENT patients for Hearing test? We have ENT who are seeing patients virtually but would like us to test these patients. Need clarity on which patients should absolutely be tested via ENT, please?
- Is there any news if DMO1 /RTT is going to be abolished/changed?
- Would be grateful for some feedback when talking about restarting services – is it the adult population you are mainly referring to, as the latest guidance I have seen is that children routine appointments are still not be done?
Shared comments/opinion
“We are seeing routine patients now – limited numbers to keep footfall low and social distancing in waiting room.”
“The limiting factor of returning to seeing routine patients is waiting area capacity (often shared with other specialities including ENT) – even when use is being made of telephone liaison and escorting patients directly to the department. Is a Trust (organisation) issue rather than Audiology.”
“For interest, NHS Scotland’s National HCS Network is restarting as of next week and at NHS Board level while it remains the individual Boards responsibility as to when it re-starts local HCS Committees and Professional Committees this in some areas is now also underway.”
“NHS Scotland has revisited it’s recent national workforce plan and asked us all in Scotland to gaze into our crystal balls to answer some thoughts and questions on where the workforce discussion should go over the coming months and year. Very difficult to do (in my opinion) so I’m not particularly comfortable that this early in the crisis we’re potentially trying to re-write or predict workforce requirements. For Physiological Science disciplines, in particular, we were in dire straights pre covid so where we will be coming out the other end is anyone’s guess BUT what I DON’T believe will change is that we’ll not see any additional investment in general in this staff group so it will continue to be challenging albeit our activity levels will be significantly reduced for some time to come which may mask the issues around a lack of people in training etc.”
Resources
NCA North East Sector Audiology Service
Questions
- Is there any advice about use of headphone covers for hearing assessments?
- Has there any guidance about sanitising hearing aids?
- I am really interested in the need to remove hearing aids prior to having a temperature check – do we know how long the hearing aid has to be removed prior to the check?
Shared comments/opinion
“Puretone do headphone covers.”
“Wiping the cushions with Clinell wipes is ok – but just be careful of a build-up of residue of the wipes on the headphone grill itself, this ultimately affects your headphones calibration. Therefore covers may be better long term?”
“Universal Clinell wipe for 6-0 seconds should kill 99.999% of lots of things including COVID. See Clinell website.”
“Hearing aid removal for temp checks: 20 mins is needed. There are some references online for this. An aid can raise the temperature by 0.8deg C.”
“AZO wipes between patients and actichlor at the end of the day.”
Resources
Questions
- Interested in the click and post service via the internet, how does that work?
- Are the AccuRx consultations video consultations?
Shared comments/opinion
“Consumables available to order from NHS website.”
“Yes – AccuRx Fleming.”
Resources
Questions
- Has anyone been using hearing self-screens for pts and established their reliability?
Shared comments/opinions
“Hearing self-screens for pts -we are currently doing a small study on 3 of them.”
Resources
Support documents
During our Heads of Service webinars, areas of interest and further support have arisen. BAA Board has looked at these different topics and compiled further information to support Heads of Service and fellow team members. Also included below are all the documents discussed during the webinars.
As Heads of Service and Service leaders, we have to look after the health and wellbeing, including mental wellbeing, of all our teams in these unprecedented times. We have had very little time to react to this but there have been some really useful suggestions for all that came out of the BAA HOS meeting. Please download the Health and Wellbeing document for ideas and support sites.
At the first Heads of Service meeting specifically addressing Covid-19, many common themes arose and heads of service shared suggestions about how they were continuing to provide routine service provision.
Although services have stopped seeing patients face-to-face unless considered urgent, everyone felt that maintaining access to good hearing for our patients was essential. However, at the time of the meeting, guidance from local employers was variable, particularly about the use of PPE.
Most services were continuing to provide a basic service using a skeleton staff, e.g. with a manager, one audiologist and one admin. Many staff are working at home and it was suggested that it would be useful to have a central list of potential tasks to be allocated. It was reported that some audiologists were already being redeployed. Many services are carrying out phone review/ follow-ups or even video reviews wherever possible and providing a postal service for consumables and hearing aids. Some useful experience was shared:
Basic audiometry
Overall most face to face activity had stopped except for some urgent ABR referrals (eg for post meningitis or high-risk NHSP referrals and urgent ENT testing. PPE was starting to be used but this was highly variable between trusts.
Hearing aid fitting
It was suggested that where audiometry had been done, hearing aids could be posted out, fitted to coupler targets with fitting done by video link, although care would need to be taken which cases were considered for this, probably not open fits.
This raised a query about how tubing would be cut to the correct length, or open fits sized if sending hearing aids and moulds as a first fit.
One service was considering posting out personal listeners as a “last resort”.
Batteries
Most services were sending batteries by post, but there were questions from some about post office policy re batteries in the post.
There was a consensus that this was allowed especially if padded envelopes were used.
Impressions
There were questions about whether impressions should be taken for only “urgent” cases (eg. for a newly diagnosed baby with a profound hearing loss) or not at all. There was a general consensus that impression taking was still being done if considered urgent/ essential. However, there was some discussion about the safety of impression taking and the use of PPE and very variable local policy at the time.
Replacement earmoulds
Some services were able to request these to be reprinted from scans by their earmould manufacturers.
For growing babies and children, it was suggested that audiologists request double-dipping and ask for 2-3% to be added on to the previously scanned impression. Alternatively, earmould manufacturers may be willing to use an existing earmould to make another one larger “double-dipped” mould for a baby or infant if the parents are willing to send in a single earmould so their baby is not without amplification.
To post out, it was suggested that registered post should be used for moulds, but standard for thin tubes (easier to replace if not delivered, but rarely an issue).
Hearing aid repairs/ postal services
Most services were offering a postal service for repairs and replacements. There were questions about whether registered post should be used, as there was concern about the potential cost of hearing aids lost in the post. Those that did use registered post found it cost-effective. However, most services did not have the facility to do this and were using standard and accepting the risk. Several heads of service who have introduced postal repairs have waived the charge for lost aids. More expensive items, such as BAHAs, tended to be posted by registered post.
Currently, some services were expecting staff to deliver earmoulds. One service reported that they were using the staff who normally do home visits to do doorstep drop-offs.
Overall, there was a very clear message from Heads of Service attending the meeting that although routine care was severely restricted, Audiology services were still determined to provide essential services (#StillHereForYou), whilst adhering to local policy and guidance. More recently, in an open letter, BAA has encouraged services to contact their CCG to reassure them that they are still able to provide these essential services to their patients.
Download the document: Essential Routine Services
BAA guidance on registration and implications for redeployment COVID-19
This guidance focuses on supporting graduates in 2020 as well as encouraging clinicians to join a PSA accredited register to ensure their practice is protected.
Supporting audiology graduates in 2020
Measures to curb the spread of COVID-19 has impacted the final year of students in various ways and universities are working hard to support students in completing their studies. This is to ensure they can progress to graduation and join the workforce. The transition from student to clinician may be different in this year and the hope is that the impact of COVID-19 should not affect their employability. One regulator has suggested that new employees complete a CPD portfolio that could be tailored to areas that they feel they could develop more. The expectation is that they should submit this CPD portfolio one year after registering. It is also advised that new graduates should be encouraged to join local or national preceptorship programmes.
Supporting unregistered staff to join an accredited register during COVID-19
Registration in Audiology is complex and currently, clinicians have a choice depending on their qualification. More information can be found here: Registration in Audiology.
The CSO produced guidance for the redeployment of staff during COVID-19 for NHS England advising that all Healthcare Science staff not currently registered are expected to join an Accredited Voluntary Register (see pg 9). Both AHCS and the RCCP are PSA accredited registers and listed in the document.
There are three organisations that hold registers which have been accredited by the Professional Standards Authority (PSA) that healthcare science professionals can join if they meet the required criteria: The Academy for Healthcare Science (AHCS), Register of Clinical Technologists (RCT) and Registration Council for Clinical Physiologists (RCCP).
The call to join a register is intended for practice to be protected within the regulatory guidelines, as all regulators are aware that clinicians may be asked to take on new roles. Regulators advise that appropriate training must be provided should clinicians be asked to work outside of regular practice. Being registered means that clinicians have a specific, identified remit of work allowing registrants to indicate when roles are outside of their practice. If they remain unregistered they could potentially be classed as part of the greater HCS workforce. The advice to register applies to all 4 home countries as regulators function in England, Northern Ireland, Scotland and Wales.
More COVID specific guidance can be found here: RCCP and AHCS
Which register to join depends on qualification and route of entry into the profession, as well as employment. Some clinicians may have more than one choice where others might be limited to one.
Please contact Lizanne Steenkamp on lsteenkamp@qmu.ac.uk if you have any questions about which register to join but also read the full guidance here.
If you’re in practice but not registered, it’s more important now than ever…
CSO Deploying the HCS workforce
Project Nightingale Audiology Skill Set
EoE Audiology Deployment Matrix
Adam Beckman has kindly shared two documents that his NHS department uses in relation to Remote Programming:
