Cochlear Implant Champions
Cochlear Implant Champion Scheme
The Cochlear Implant (CI) Champion scheme is a joint initiative with BAA and BCIG and was launched in 2019. The aim of the scheme is to ensure that all eligible adults and children, and their families, are well-informed about cochlear implants and are offered a timely referral.
——————————
Why do we need the scheme?
The referral guidelines have widened, benefits demonstrated, and yet those with a CI remain low!
- CI recipients experience improvements compared with hearing aid only or no treatment, in terms of: speech perception, educational and employment opportunities, and quality of life
- CIs have been shown to be cost effective
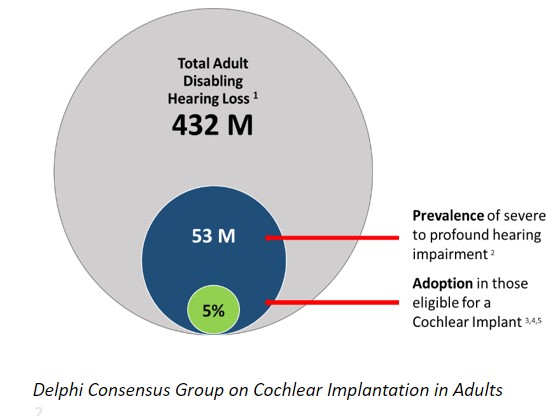
- However, use of CIs in eligible adults is as low as 5% globally* and predicted to be as low as 7% in the UK
- Duration of hearing loss before CI is increasing over time
- Low awareness of CI as a treatment option
- Low awareness of CI candidacy criteria
——————————
How can the CI Champion Scheme help?
- Improve communication between referring and implant teams
- Promote shared care between teams to ensure patients have a smooth and timely transition from HA to CI (if they want it).
- Audit, to understand training needs and drive changes in clinical practice.
- Training focussing on candidacy and referral
- Peer-support to help colleagues develop and revaluate their practice.
- A national change, driven by referring audiologists.

Our aim is to have a CI Champion in every UK Audiology Department, both adult and paediatric, and both NHS and Private. Their local CI Mentor supports the CI Champions in their local CI Centre.
Click on the boxes below to discover more information about the different areas of the scheme.
